Supporting physician decision making
Project Overview
MICA’s Center for Social Design
[Practice-Based Studio]
Year: 2019
Project team:
[Instructor] Becky Slogeris
[Associate] Cameron Morgan
[Student] Eunsoo Kim, Sasha Avrutina, Kadija Hart, Vidisha Agarwalla, Eesha Patne, Ayangbe Mannen, Harley French
Collaborating with: Johns Hopkins School of Medicine
My role on this project: research, interviews, Final prototype
About the project
The Connected Emergency Care (CEC) Patient Safety Learning Lab (PSLL) is a joint effort between MICA’s Center for Social Design and Johns Hopkins Medicine to reduce health and financial harm caused by a disconnected emergency care system. The five-year, longitudinal project will include multiple studios through the Center to generate solutions which are informed, user-centric and effective for practitioners and patients. The solutions generated will be implemented at two campuses: in Baltimore City (JHH) and Howard County (HCGH).
The initial focus will be on problems related to patients with suspected lower respiratory tract infection (LRTI), a leading cause of emergency room (ER) admissions and deaths. LRTI vary widely in the way they present in patients, making diagnosis and treatment difficult. The tensions in diagnosis and treatment are exacerbated by the following factors:
The absence of a longitudinal relationship between clinician and patient results
Missing clinical and social contextual information during important decision making junctures
Post-encounter feedback about downstream patient care events are rarely seen, limiting outcome-driven decision making and continuous learning
ER crowding, which creates a hazardous decision-making environment fraught with time- pressure and high caseloads
These factors perpetuate a disconnected, open-loop system where measures of output (patient outcomes and cost) have limited effect on input (physician decision-making). In partnership with the PSLL team and other stakeholders, MICA’s Center for Social Design will work better understand barriers to informed decision making and develop design prototypes with the ultimate goal of creating a closed feedback loop to better support physician decision making.
Design Challenge
“How might we create a closed feedback loop with post-encounter data to better support physician decision making?”
Human-Centered Design
The project team utilized a human-centered and collaborative process to understand and define problems, identify opportunities and generate ideas, and make tools that support physician decision making.
Research Recap
In a close partnership with Johns Hopkins Hospital, physicians provided a background on the Emergency Department (ED) ecosystem and the current situation that leads them to lack post-encounter patient information. They shared with us a dashboard that emergency physicians use in their daily practice. We also supplemented this information by reading about emergency medicine, physician decision making, ED culture, as well as AI & data science. This led us to three guiding questions that helped us throughout the research phase.
Guiding Questions
What information is important and constructive for physicians?
What information and feedback do physicians currently base their decision making on?
How might we design incoming feedback/info and supporting systems to ensure the tool is used?
Methods
Secondary research, interviews, surveys, shadowing
Interview & Survey Summary
Interviews
We visited Howard County General Hospital and the Johns Hopkins Hospital to observe the ED environment and interview physicians. We talked to 15 physicians and shadowed them to immerse ourselves in the environment.
Surveys
We conducted a survey with 24 attending physicians to better understand their needs and desires for patient feedback and follow-up. Through surveys, we could understand what information ED physicians want to know with patients and the levels of information.
Synthesis
The information collected from interviews and observation was themed into categories. We found interesting tensions among datas and gained insights from them. Next, we developed four opportunity questions to generate ideas.
Physician Personas
We developed personas of ED physicians as a way to ensure a full spectrum of personalities and work-styles are considered when going to brainstorming ideas. These characters were created based on a synthesis of data collected from interviews and surveys. Each persona reveals bright spots (+) and pain points (-). No one persona is based on just one person—instead, each persona is an amalgamation of multiple individuals.
Design Principles
Next, we developed six design principles based on what we learned from the research. Together, the design principles formed a framework to guide the team through the rest of the HCD process, through ideation, prototyping, and implementation.
Ideation
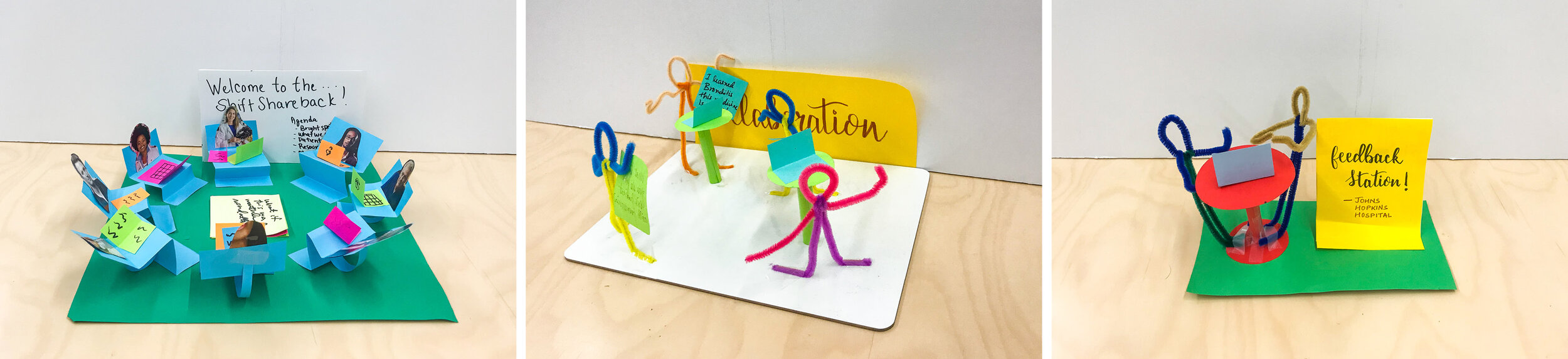
The team facilitated a shareback session where physicians and other stakeholders from Johns Hopkins were invited to get an update on our progress and participate in ideation. They reviewed the themes, insights, and opportunities to generate ideas. At the end of the session, physicians and stakeholders, along with the MICA team, created a movie trailer to describe our ideas and act out. This exciting environment encouraged people to think of creative ideas.
Prototype
The team gathered the ideas from brainstorming session and organized them into categories. Each team member developed prototypes based on the categories. These low-fidelity mock-ups ranged from analogous ideas to digital systems. These prototypes were then shared with our partners for feedback.
1. Persona-based and customized dashboard
2. Screen design and specific features of the dashboard
3. Collaboration Activities
After considering the feedback from our partners at Johns Hopkins, we narrowed down the prototypes to focus on the design of a digital dashboard.
Final Idea: Digital Dashboard
A digital dashboard would improve internal and external physician communication around patient statuses and diagnosis. In addition, the dashboard would offer a variety of customizable features to meet each physician’s specific needs in an effort to maximize their efficiency and improve their decision-making skills.
The dashboard was inspired by our design challenge to create a closed feedback loop that would better support physician decision making while assisting patients in the Emergency Department.
Experience Map
An experience map is a visualization that captures the experience of the dashboard across touch points. It includes four stages from reaching out to physicians to incorporating learnings to practice.
Final Shareback Session
The team facilitated a final shareback session of our progress to get input on our feature bucket and experience map. Two activities were developed to guide the feedback session.
Final Prototype
“If feedback is given in a couple of days, we will possibly minimize the number of decision-making errors.”
After finishing the class, I developed the dashboard’s UI design based on the physicians’ feedback. This prototype includes specific features that ED physicians want to have and supports them throughout design making. It shows critical data about patients’ outcomes after being discharged. ED physicians can pin each patient’s information and follow up with them later on. They are also able to review their diagnosis and treatment to improve overall outcomes. Underneath the patient’s lists, a progress bar will help patients receive treatment in a timely manner.
“If I have a tendency of making a mistake, I would like to know before the mistake occurs.”
Many ED physicians find difficulties in looking for patients’ outcome. They want to look through all the data quickly and review it thoroughly at the same time. This prototype is designed to give a specific search function, which narrows down the data while presenting detailed information on the patient they’re looking for.
Project team photo